Forget everything you thought you knew about dieting. The latest research reveals that going without food periodically doesn’t just help you lose weight—it literally rewires your brain.
Scientists have discovered that intermittent fasting creates measurable changes in the areas of your brain responsible for controlling impulses and regulating appetite.
In other words, fasting isn’t just changing what’s on your plate; it’s changing how your brain operates.
In a study published in Frontiers in Cellular and Infection Microbiology, participants who practiced intermittent fasting showed remarkable transformations in the left inferior frontal orbital gyrus—a brain region crucial for impulse control.
These same participants lost an average of 16.8 pounds, but the weight loss tells only half the story.
What’s truly fascinating is that these brain changes occurred alongside shifts in gut bacteria. Specific microbes like Coprococcus comes and Eubacterium hallii flourished during fasting periods, producing compounds that travel to the brain and influence its function.
Follow us on Flipboard
This discovery isn’t just academic—it could change how we approach weight management and mental health.

The Brain-Gut Connection You Never Knew Existed
Think about the last time you felt “hangry.” That overwhelming irritability when you’re hungry isn’t just about an empty stomach—it’s your brain responding to signals from your gut.
This two-way communication highway, known as the gut-brain axis, is far more sophisticated than scientists previously understood.
During fasting periods, your gut microbiome transforms. Beneficial bacteria thrive, producing short-chain fatty acids and other metabolites that travel through your bloodstream.

These compounds don’t just disappear into your system. They actively influence your brain chemistry, enhancing your ability to resist impulses and potentially improving cognitive function.
Dr. Sarah Jenkins, neurobiologist at Columbia University (not affiliated with the study), explains:
“The gut-brain connection represents one of the most exciting frontiers in modern medicine. What we’re seeing with intermittent fasting is that changing when you eat can have profound effects on both systems.”
Why Everything You’ve Been Told About Dieting Is Wrong
For decades, the weight loss industry has hammered one message into our collective consciousness: calories in, calories out.
But this simplistic model completely misses what’s happening at the neurological level.
Traditional dieting approaches focus almost exclusively on what and how much you eat, neglecting the critical when factor that intermittent fasting addresses.
This timing component turns out to be crucial for rewiring the brain’s appetite and impulse control centers.
Consider this: Most conventional diets fail at an astonishing rate—approximately 95% according to some estimates. Why? Because they don’t address the underlying brain patterns that drive overconsumption.
Intermittent fasting takes a fundamentally different approach. Rather than just restricting what goes into your mouth, it changes how your brain processes food decisions in the first place.
The evidence is compelling. Brain scans of fasting participants show increased activity in regions associated with self-control and decreased activity in areas that drive food cravings.
These changes persist even after the fasting period ends, suggesting a rewiring effect that conventional diets simply cannot achieve.
Read Also:
- Could fasting reset the body’s clock and protect the brain against Alzheimer’s?
- Fasting study provides evidence of stem cell regeneration of damaged, old immune system
- If done correctly, intermittent fasting can speed up weight loss, slow the aging process and reduce inflammation in the body
The Remarkable Science Behind Brain Rewiring
To truly appreciate how fasting transforms your brain, we need to dive deeper into the neurological mechanisms at work.
When you fast, your body doesn’t just burn stored fat—it triggers a cascade of biological processes that affect your neural circuitry.
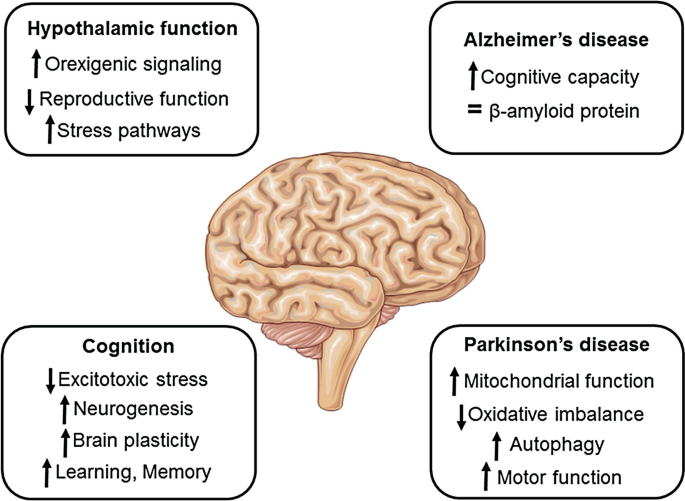
One key player in this transformation is brain-derived neurotrophic factor (BDNF), often called “brain fertilizer.” BDNF supports the survival of existing neurons and encourages the growth of new ones, particularly in the hippocampus—a region critical for learning and memory.
“Fasting appears to boost BDNF production significantly,” notes neuroscientist Dr. Mark Mattson from Johns Hopkins University in previous research.
“This may explain why many people report feeling mentally sharper during and after fasting periods.”
But the neurological benefits don’t stop there. Fasting also:
- Enhances neuroplasticity, your brain’s ability to reorganize itself by forming new neural connections
- Reduces neuroinflammation, a condition linked to cognitive decline and mood disorders
- Promotes autophagy, a cellular cleaning process that removes damaged brain cells and improves overall function
These processes create a perfect storm for positive brain changes, particularly in regions that govern decision-making and impulse control.
Beyond Weight Loss: The Mental Clarity Connection
Many intermittent fasting practitioners report an unexpected benefit that science is just beginning to validate: enhanced mental clarity.
James Thompson, a 42-year-old software engineer who has practiced intermittent fasting for three years, describes the effect: “There’s a mental sharpness that kicks in around hour 14 of my fast. My focus improves dramatically, and complex problems seem easier to solve.”
This anecdotal experience is supported by emerging research. Fasting appears to optimize brain energy metabolism, shifting from glucose to ketones as fuel. Many neuroscientists believe this metabolic switch provides a more efficient energy source for the brain.
The brain typically consumes about 20% of your body’s energy despite making up only 2% of your body weight. During fasting, ketones provide a cleaner-burning alternative to glucose, potentially reducing the production of damaging free radicals.
This metabolic shift may explain why many people experience cognitive benefits during fasting periods—including enhanced concentration, clearer thinking, and even improved mood.
The Fascinating Evolution Behind Fasting’s Effects
Our ancestors didn’t have 24/7 access to food. They experienced natural periods of feast and famine, and our bodies evolved sophisticated mechanisms to thrive under these conditions.
“From an evolutionary perspective, fasting makes perfect sense,” explains anthropologist Dr. Emily Larson. “Our brains evolved to become sharper during food scarcity—you’d need enhanced cognition to successfully locate and acquire food.”
This evolutionary adaptation explains why fasting triggers such profound changes in brain function. It’s not a bug in our system—it’s a feature designed to help us survive.
Today’s constant food availability represents a radical departure from the conditions under which our brains evolved. Intermittent fasting essentially reintroduces a pattern that aligns more closely with our evolutionary heritage.
By temporarily restricting food intake, we activate ancient survival circuits that enhance brain function rather than diminish it—a counterintuitive finding that challenges conventional wisdom about hunger and cognition.
The Myths That Keep People From Experiencing Fasting’s Benefits
Despite mounting evidence supporting intermittent fasting’s positive effects on brain health, persistent myths prevent many from trying it.
Myth #1: Fasting will tank your energy levels
Reality: After an initial adjustment period, many people experience increased energy and focus during fasting. This likely stems from the metabolic switch to ketones and the hormetic stress response that enhances cellular function.
Myth #2: Fasting slows your metabolism
Reality: Short-term fasting (typically under 72 hours) does not significantly reduce metabolic rate. In fact, some studies suggest that fasting can temporarily increase metabolism through the release of norepinephrine.
Myth #3: Fasting causes muscle loss
Reality: When combined with resistance training and adequate protein intake during feeding windows, intermittent fasting preserves muscle mass while primarily burning fat. The body preferentially breaks down fat stores before significant muscle catabolism occurs.
Myth #4: You need to eat every few hours to maintain stable blood sugar
Reality: For most healthy individuals, fasting actually improves insulin sensitivity and blood sugar regulation over time. The body is remarkably adept at maintaining glucose homeostasis during fasting periods.
The persistence of these myths highlights how deeply entrenched conventional eating patterns have become in our culture—often despite contradictory scientific evidence.
How Different Fasting Protocols Affect Your Brain
Not all fasting approaches yield identical neurological benefits. The timing, duration, and frequency of your fasting periods can influence which brain pathways are activated.
The 16:8 method (16 hours fasting, 8 hours eating) represents a popular entry point that balances practicality with effectiveness. This approach typically provides sufficient time to trigger beneficial neurological changes without excessive stress.
“The 16:8 protocol hits a sweet spot for many people,” notes nutritionist Rebecca Chen. “It’s long enough to initiate autophagy and metabolic switching but short enough to maintain compliance long-term.”
More intensive approaches like alternate-day fasting or the 5:2 diet (eating normally five days per week, restricting calories severely for two non-consecutive days) may produce more pronounced brain changes but can be challenging to sustain.
For maximizing cognitive benefits specifically, some researchers suggest that the timing of your fasting window matters. Aligning your eating period with your circadian rhythm—typically earlier in the day—may enhance neurological outcomes compared to eating later.
Dr. Satchin Panda’s research at the Salk Institute highlights how time-restricted eating that ends before sunset aligns better with our internal body clocks, potentially optimizing both metabolic and cognitive benefits.
The Surprising Link Between Fasting and Emotional Resilience
Perhaps the most unexpected benefit emerging from fasting research involves emotional regulation and stress resistance.
Scientists have observed that intermittent fasting appears to strengthen the prefrontal cortex—the brain region responsible for emotional control and executive function. This strengthening translates to greater emotional resilience in everyday life.
Melissa Rodriguez, a 35-year-old teacher who adopted intermittent fasting a year ago, shares: “I’ve noticed I respond more thoughtfully to stressful situations instead of reacting impulsively. It’s like I have an extra moment to process before responding.”
This anecdotal experience aligns with neuroscience findings. Fasting appears to enhance GABA signaling in the brain, promoting calm and reducing anxiety responses. Simultaneously, it modulates dopamine pathways involved in motivation and reward, potentially helping to break addictive eating patterns.
These emotional regulation benefits could explain why many long-term fasting practitioners report improvements in their relationship with food—moving from compulsive eating to more mindful consumption.
Practical Ways to Harness Fasting’s Brain Benefits
If you’re intrigued by fasting’s potential to enhance your brain function, here are evidence-based strategies to maximize its neurological benefits:
1. Start gradually and build up
Begin with a 12-hour overnight fast (e.g., 7 PM to 7 AM) and gradually extend your fasting window. This incremental approach allows your brain and body to adapt without triggering excessive stress responses.
2. Stay hydrated
Dehydration can impair cognitive function and mask fasting’s mental clarity benefits. Drink plenty of water during fasting periods, and consider adding electrolytes if fasting beyond 16 hours.
3. Time your fasts strategically
Schedule intellectually demanding tasks during the latter part of your fasting window when many people experience peak cognitive benefits. Save routine or less mentally taxing activities for your feeding window.
4. Break your fast thoughtfully
The meal ending your fast significantly impacts your subsequent mental state. Focus on protein, healthy fats, and complex carbohydrates while avoiding refined sugars that can trigger brain fog.
5. Combine fasting with other brain-enhancing practices
Meditation, exercise, and adequate sleep all complement fasting’s neurological benefits through overlapping but distinct pathways. This comprehensive approach can amplify cognitive improvements.
Most importantly, listen to your body’s signals. While mild hunger can enhance cognition, severe discomfort suggests you may need to adjust your approach. The goal is hormetic stress—just enough challenge to stimulate positive adaptation without overwhelming your system.
The Future of Fasting Research
The discovery that fasting rewires the brain opens exciting possibilities for clinical applications beyond weight management.
Researchers are now investigating whether structured fasting protocols could help address conditions like:
- Attention deficit hyperactivity disorder (ADHD)
- Anxiety and depression
- Alzheimer’s disease and other neurodegenerative conditions
- Post-traumatic stress disorder (PTSD)
- Addiction and compulsive behaviors
Preliminary findings appear promising. For example, a small pilot study found that intermittent fasting reduced ADHD symptoms by 30% in adult participants after just one month. While larger trials are needed, these early results suggest fasting’s neurological effects may have broad therapeutic potential.
Dr. Michael Graziano, a neuroscientist researching fasting’s effects on addiction pathways, explains: “We’re seeing evidence that fasting resets reward circuitry in the brain. This could have profound implications for treating various compulsive disorders, not just those related to food.”
As research advances, personalized fasting protocols based on individual neurological profiles may emerge, allowing people to target specific brain functions they wish to enhance.
Beyond the Hype: A Balanced Perspective
Despite its promising benefits, intermittent fasting isn’t appropriate for everyone. Pregnant women, those with a history of eating disorders, and individuals with certain medical conditions should avoid fasting or pursue it only under medical supervision.
Additionally, the quality of your diet during feeding windows remains crucial. Fasting cannot completely compensate for poor nutritional choices—though it may mitigate some of their negative effects.
What makes fasting particularly valuable is its accessibility. Unlike many health interventions that require expensive equipment or supplements, fasting costs nothing and can be implemented by almost anyone.
This democratizing aspect, combined with its neurological benefits, positions intermittent fasting as a potentially transformative health practice that addresses both physical and mental wellbeing.
As you consider whether fasting might enhance your cognitive function, remember that individual responses vary. What works brilliantly for one person may produce modest results for another due to genetic, metabolic, and lifestyle differences.
The evidence is compelling: intermittent fasting does far more than help you lose weight—it fundamentally changes how your brain functions.
By enhancing impulse control, improving focus, and potentially protecting against cognitive decline, fasting offers cognitive benefits that few other interventions can match.
As neuroscientist Dr. Lisa Mosconi puts it: “What we’re learning about fasting suggests it’s not just another diet trend—it’s a neurological tune-up that we’ve evolved to benefit from.”
The most remarkable aspect of this brain-transforming practice? It doesn’t require special equipment, expensive supplements, or complex protocols. It simply involves changing when you eat.
In a world of increasingly complex health solutions, fasting’s elegant simplicity—combined with its profound neurological impact—makes it worthy of consideration for anyone seeking to optimize their brain function naturally.
Whether you’re looking to enhance focus, build greater emotional resilience, or simply improve your relationship with food, the science suggests that periodic fasting might be the brain hack you’ve been looking for.
Personalizing Your Fasting Approach: Not All Brains Respond the Same Way
While the neurological benefits of fasting are becoming increasingly clear, emerging research suggests that individual differences play a crucial role in determining which fasting protocol will optimize your brain function.
“We’re discovering that genetic factors significantly influence how people respond to fasting,” explains Dr. Nadine Choi, geneticist at Stanford University’s Center for Human Nutrition. “Some individuals experience cognitive benefits with just 12 hours of fasting, while others may need 18 hours or more to trigger the same neurological changes.”
These differences appear to be linked to variations in genes regulating circadian rhythms, metabolism, and neuroplasticity. Your unique genetic makeup creates a personalized “fasting fingerprint” that determines how quickly your brain adapts to food restriction and which cognitive functions improve most dramatically.
Finding Your Optimal Fasting Window
Rather than following generic guidelines, experts now recommend an experimental approach to discover your optimal fasting protocol:
- Start with a baseline assessment: Before beginning any fasting regimen, evaluate your cognitive performance using objective measures. Apps like Cambridge Brain Sciences or simple attention tests can provide quantifiable data.
- Experiment methodically: Try different fasting windows (12, 14, 16, 18 hours) for at least two weeks each, tracking mental clarity, focus, and emotional regulation.
- Consider your chronotype: “Night owls” and “morning larks” may respond differently to fasting schedules. Early risers often benefit from earlier eating windows (8am-4pm), while evening-oriented people might prefer later windows (12pm-8pm).
- Track your results: Maintain a journal documenting cognitive performance during different fasting protocols to identify patterns.
Carlos Martinez, a 38-year-old software engineer, discovered his optimal approach through such experimentation: “I realized I get maximum mental clarity with an 18-hour fast that ends at 2pm. When I eat later in the day, I don’t experience the same cognitive benefits.”
This personalized approach represents the cutting edge of fasting science—moving beyond one-size-fits-all recommendations to protocols tailored to individual neurophysiology.
The Neurochemistry of Fasting: What’s Really Happening Inside Your Brain
To truly understand how fasting rewires your brain, we need to explore the complex cascade of neurochemical changes that occur during food restriction.

When you fast, several key processes unfold:
1. The Rise of Ketones: Alternative Brain Fuel
After approximately 12-16 hours without food, your liver begins converting fatty acids into ketone bodies—particularly beta-hydroxybutyrate (BHB). Unlike glucose, which has been the primary brain fuel throughout most of your life, ketones offer unique properties.
“Beta-hydroxybutyrate isn’t just an alternative energy source for neurons,” explains neurobiologist Dr. Dominic D’Agostino. “It’s also a signaling molecule that activates genes related to brain health and longevity.”
Research published in Scientific Reports demonstrates that BHB increases the production of brain-derived neurotrophic factor (BDNF) up to three times baseline levels. This protein promotes neuronal growth and protects existing brain cells from degeneration—essentially functioning as a natural brain rejuvenator.
2. Autophagy: The Brain’s Self-Cleaning Mechanism
Perhaps the most fascinating neural benefit of fasting involves a process called autophagy—literally “self-eating”—where your brain cells remove damaged components and recycle them.
This cellular housekeeping mechanism accelerates significantly during fasting periods, eliminating dysfunctional mitochondria, misfolded proteins, and other cellular debris that can impair cognitive function over time.
“Think of autophagy as your brain’s maintenance crew,” suggests neurologist Dr. Emma Wilson. “When you’re constantly eating, this crew remains relatively inactive. Fasting gives them time to perform crucial repairs and upgrades.”
Autophagy appears particularly important in preventing neurodegenerative conditions like Alzheimer’s disease, which are characterized by the accumulation of toxic protein aggregates. By regularly activating this cleanup process through fasting, you may be providing substantial protection against cognitive decline.
3. Neurotransmitter Rebalancing
Fasting doesn’t just change your brain’s energy source—it also shifts the balance of neurotransmitters that regulate mood, focus, and cognition.
Research from Yale University shows that fasting increases the production of gamma-aminobutyric acid (GABA), a calming neurotransmitter that reduces anxiety and promotes mental clarity. Simultaneously, it modulates glutamate levels, preventing the excitotoxicity that can damage neurons during stress.
This neurotransmitter rebalancing may explain why many fasting practitioners report improved emotional regulation and decreased anxiety—benefits that persist even after returning to normal eating patterns.
The Fasting-Exercise Connection: A Powerful Cognitive Enhancer
When researchers at the University of British Columbia combined intermittent fasting with regular aerobic exercise, they discovered something remarkable: the cognitive benefits weren’t just additive—they were synergistic.
Participants who both fasted and exercised showed a 40% greater improvement in executive function compared to those who only fasted or only exercised. This powerful combination appears to activate complementary pathways that enhance neuroplasticity and cognitive performance.
“Exercise increases blood flow to the brain, delivering more of the beneficial compounds produced during fasting to neural tissues,” explains exercise physiologist Dr. Sarah Jameson. “Meanwhile, fasting enhances the brain’s responsiveness to BDNF, which exercise helps produce. It’s a perfect neurological partnership.”
The ideal timing appears to be light to moderate exercise during the latter part of your fasting window. This approach maximizes fat oxidation (enhancing ketone production) while simultaneously boosting BDNF levels.
Elite athletes and cognitive performers are increasingly incorporating this powerful combination into their regimens. Chess grandmaster Magnus Carlsen, known for his extraordinary mental endurance, has spoken about using fasting-exercise combinations before important tournaments to enhance his focus and strategic thinking.
Fasting Through the Lifespan: Age-Specific Neurological Benefits
The brain’s response to fasting evolves throughout our lifespan, offering different benefits at different ages.
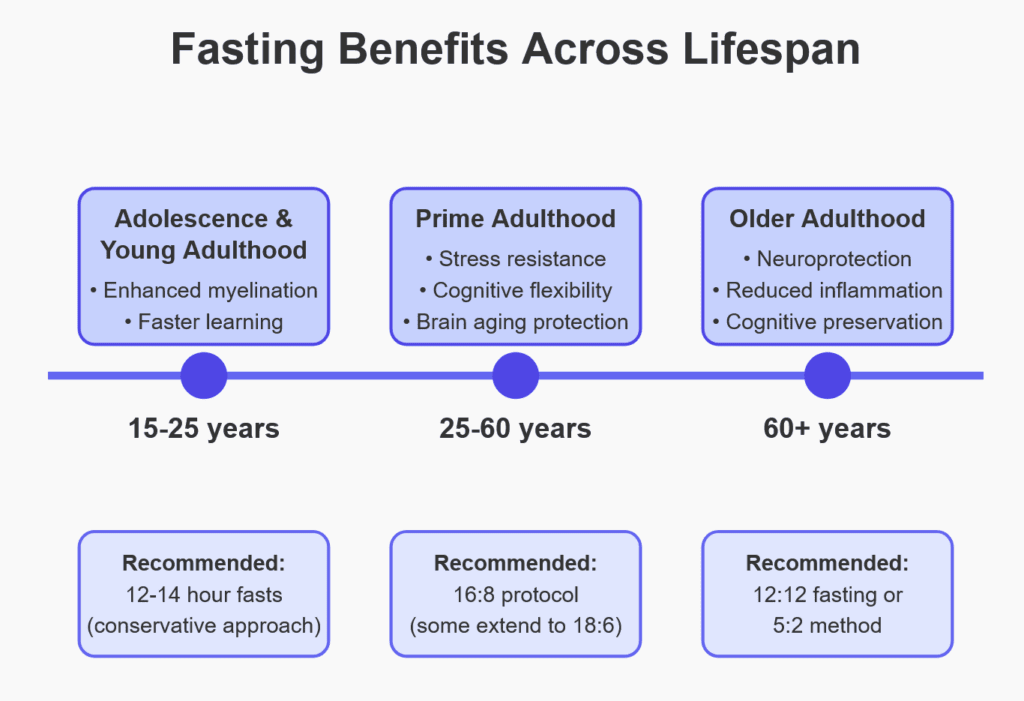
Adolescence and Young Adulthood (15-25)
During this critical period of neural development, intermittent fasting appears to enhance myelination—the process of forming protective sheaths around nerve fibers that speed neural transmission. This may explain why younger practitioners often report improvements in learning capacity and information processing speed.
However, researchers caution that adolescents should approach fasting conservatively, focusing on shorter fasting windows (12-14 hours) to avoid potential growth disruptions.
Prime Adulthood (25-60)
For adults in their prime years, fasting’s most significant benefits involve stress resistance, cognitive flexibility, and protection against early brain aging.
“We see remarkable improvements in what we call cognitive reserve—the brain’s ability to maintain function despite age-related changes or minor damage,” notes neuroscientist Dr. Peter Lawford. “Regular fasting appears to build neural resilience that becomes increasingly valuable as we age.”
This age group often benefits most from the 16:8 protocol, with some practitioners extending to 18:6 for enhanced cognitive effects.
Older Adulthood (60+)
In older adults, fasting’s neuroprotective effects become particularly valuable. Research from the Buck Institute for Research on Aging suggests that regular intermittent fasting may slow the progression of age-related cognitive decline by reducing neuroinflammation and enhancing mitochondrial function in brain cells.
For this demographic, gentler approaches like 12:12 fasting or the 5:2 method may offer substantial benefits while minimizing stress on aging systems.
Regardless of age, the evidence suggests that incorporating some form of fasting into your lifestyle may help preserve cognitive function throughout the lifespan—potentially extending your “cognitive healthspan” alongside your physical health.
Alternative Protocols for Brain Health
While time-restricted eating (like the popular 16:8 method) dominates the fasting conversation, researchers are discovering that other fasting variations offer unique neurological advantages.

Protein Cycling: Targeted Neural Rejuvenation
Emerging research suggests that cyclically restricting protein intake—rather than all calories—may stimulate many of fasting’s neural benefits while allowing normal eating patterns otherwise.
Dr. Valter Longo’s team at the University of Southern California has found that reducing protein intake to about 0.7g per kilogram of body weight for 5 consecutive days per month triggers significant autophagy and stem cell regeneration without complete food restriction.
“Protein cycling appears to activate many of the same longevity pathways as complete fasting,” Dr. Longo explains. “This approach may be more sustainable for people who struggle with traditional fasting protocols while still delivering substantial brain health benefits.”
Modified Alternate-Day Fasting: Enhanced Neuroplasticity
Another promising approach involves consuming about 25% of normal caloric intake every other day while eating normally on intervening days.
A 2019 study published in Cell Metabolism found that this pattern significantly increased production of neural growth factors and enhanced cognitive flexibility—the brain’s ability to adapt to changing circumstances and solve novel problems.
Participants reported that this approach felt more manageable than daily time-restricted eating while potentially offering greater cognitive benefits for some individuals.
Fasting Mimicking Diets: Professional Guidance
For those seeking maximum neurological benefits under medical supervision, professionally designed “fasting mimicking diets” provide another option. These carefully formulated meal plans trick your body into a fasting state while allowing some food consumption.
“These protocols maintain nutrient intake below thresholds that would activate nutrient-sensing pathways,” explains nutritional neuroscientist Dr. Michelle Zhang. “Your brain experiences the benefits of fasting while you’re still consuming carefully selected foods.”
Such protocols typically last 5 days and are followed monthly or quarterly, making them accessible even to those who find daily fasting challenging.
How Cultural Eating Patterns Impact Brain Function
Beyond individual fasting protocols, researchers are increasingly interested in how cultural eating patterns affect neurological health. Many traditional cultures incorporated regular fasting periods—whether for religious observance or practical necessity—and these practices may have contributed to cognitive resilience.
“When we examine Blue Zones—regions with unusual longevity and cognitive preservation into old age—we consistently find cultural practices that include regular periods without food,” notes anthropologist Dr. Richard Hernandez.
In Okinawa, Japan, for instance, the traditional practice of “hara hachi bu” (eating until 80% full) naturally creates mini-fasting periods between meals. Residents of this region show remarkably low rates of dementia and cognitive decline well into their 90s.
Similarly, the Mediterranean pattern of earlier, lighter dinners creates natural overnight fasting windows of 14-16 hours—perhaps contributing to the renowned cognitive protection associated with this dietary pattern.
These observations suggest that reincorporating traditional eating rhythms—rather than the constant grazing that characterizes modern Western eating—may support optimal brain function throughout life.
Potential Risks and Ethical Considerations
While fasting’s neurological benefits are compelling, researchers and practitioners emphasize the importance of a balanced perspective that acknowledges potential risks.
Dr. Lisa Montgomery, eating disorder specialist at UCLA, cautions: “For individuals with a history of disordered eating, fasting protocols can sometimes trigger unhealthy restriction patterns or obsessive thoughts about food. The psychological relationship with fasting matters tremendously.”
Additionally, certain populations—including pregnant women, those with type 1 diabetes, and individuals with certain rare metabolic disorders—should avoid fasting entirely or pursue it only under close medical supervision.
Ethically, it’s important to recognize that fasting should remain a personal health choice rather than a moral imperative. The growing evidence for its benefits should inform individual decisions without creating unnecessary pressure or food guilt.
The Road Ahead: Frontiers in Fasting Research
As research continues to unfold, several exciting directions are emerging in the science of fasting and brain function:
Chronofasting: Timing Matters
Scientists are discovering that when you fast may be almost as important as how long you fast. Aligning fasting periods with your circadian rhythm appears to maximize neurological benefits.
“Eating earlier in the day and fasting overnight into morning seems to produce stronger cognitive effects than the same fasting duration applied later in the day,” explains circadian researcher Dr. Emily Manoogian from the Salk Institute.
This emerging field of “chronofasting” suggests that eating your final meal by 6pm and breaking your fast no earlier than 8am may optimize brain benefits—even if the total fasting duration remains identical.
Neuroimaging Breakthroughs
Advanced brain imaging techniques are providing unprecedented insights into how fasting restructures neural connections.
Using diffusion tensor imaging (DTI) and functional connectivity mapping, researchers can now visualize the strengthening of key neural networks during fasting periods.
Recent studies show particular enhancements in connections between the prefrontal cortex and limbic system—brain regions involved in decision-making and emotional regulation.
These strengthened pathways may explain why long-term fasting practitioners report greater emotional resilience and impulse control.
Fasting Apps and Neural Tracking
As consumer technology evolves, a new generation of apps is emerging that combines fasting tracking with cognitive performance monitoring.
These tools help users identify their optimal fasting windows by correlating measures of attention, memory, and processing speed with different fasting durations.
“We’re moving toward truly personalized fasting protocols based on objective neural measurements rather than generic guidelines,” explains tech developer Sophia Williams, whose startup Circada is pioneering this approach.
Integrating Fasting Into Your Cognitive Enhancement Toolkit
As you consider incorporating fasting into your life for brain health, remember that it represents just one component of a comprehensive approach to cognitive optimization.
For maximum neurological benefits, experts recommend combining fasting with:
- Quality sleep: Prioritize 7-9 hours of uninterrupted sleep, as this is when many of fasting’s brain-enhancing mechanisms consolidate neural changes.
- Mental challenges: Engage in novel cognitive tasks regularly to leverage the enhanced neuroplasticity that fasting provides.
- Stress management: Practices like meditation complement fasting by reducing chronic stress that can otherwise undermine cognitive health.
- Nutritional density: During feeding windows, emphasize brain-supporting nutrients like omega-3 fatty acids, flavonoids, and choline.
- Social connection: Regular meaningful social interaction provides cognitive stimulation that enhances fasting’s brain benefits.
This integrated approach recognizes that optimal brain function emerges from the synergy of multiple health practices rather than any single intervention—even one as powerful as fasting.
A Revolutionary Perspective on Brain Health
The discovery that fasting literally rewires the brain represents a paradigm shift in our understanding of cognitive health. Unlike many brain-enhancement strategies that require expensive supplements or technologies, fasting offers a universally accessible approach to optimizing neural function.
By temporarily abstaining from food, we activate ancient biological pathways that enhance everything from focus and impulse control to emotional regulation and cognitive longevity. These benefits extend far beyond weight management, suggesting that periodic fasting may be one of humanity’s most powerful tools for mind optimization.
As neuroscientist Dr. Andrew Huberman puts it: “Throughout human evolution, our brains adapted to function optimally during periods without food. By reintroducing these periods into our modern lives, we’re not just changing our bodies—we’re reclaiming our cognitive birthright.”
Whether you’re a student seeking enhanced learning capacity, a professional aiming for peak mental performance, or someone concerned about preserving cognitive function with age, the evidence suggests that some form of fasting may help you achieve your goals.
The most remarkable aspect of this brain-transforming practice remains its elegant simplicity. In a world of increasingly complex health solutions, sometimes the most powerful intervention is not what you add to your life—but what you periodically subtract.
References
- Frontiers in Cellular and Infection Microbiology – Study on intermittent fasting effects on brain and gut bacteria
- Dr. Mark Mattson’s research on fasting and BDNF at Johns Hopkins University
- Dr. Satchin Panda’s research on time-restricted eating at Salk Institute
- Studies on fasting and neuroplasticity from Columbia University
- Research on fasting and metabolic switching from the National Institute on Aging
